Esophageal cancer is one of the top leading causes of cancer-related deaths in Malaysia. To date, neither the prevalence nor incidence of esophageal cancer nationally have been recorded. Esophageal cancer remains a major and lethal health problem even if it is not common in Malaysia. The late presentation of esophageal cancer makes it a difficult and challenging medical problem. Therefore, more governmental and non-governmental organizations in Malaysia should emphasize primary and secondary prevention strategies (reference: September 2016 – Asian Pacific journal of cancer prevention: APJCP 17(8):3705)
Esophageal cancer was commonest in Chinese ethnicity (41%), followed by Malay (29.9%), Indian (17.4%) and others (11.8%) – ( 2018 data). Esophageal Cancer disease awareness initiatives, campaigns, early detection and multimodality treatment options are essential for improved patient outcomes.
(Reference: Diseases of the Esophagus, Volume 31, Issue Supplement_1, September 2018, Page 185, https://doi.org/10.1093/dote/doy089.PS02.224)
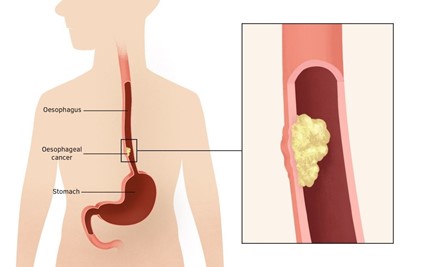
- What is esophageal cancer?
Esophageal cancer is tumour that grows in the food pipe. There are two common types of oesophageal cancer: Squamous and adenocarcinoma, which are two distinct types of cancer that carry different risk factors, biological behaviour, genetic predisposition, treatment and even prognosis.
- What causes esophageal cancer?
In general, there are two types of oesophageal cancer. The squamous cell carcinoma and the oesophageal adenocarcinoma. The former comprises 80%-90% of the cases.
Squamous cell cancer is mainly seen in heavy smokers and alcohol users; whereas adenocarcinoma is associated with reflux disease and the precursor of cancer: Barrett’s oesophagus. Other relevant risk factors for adenocarcinoma are obesity, cigarette smoking, family history, male gender, high red meat consumption and low vegetable and fruit intake.
Esophageal cancer is an uncommon cancer. It is ranked 15th and 26th among cancers in male and female respectively. (Based on 2012- 2016 National cancer registry report.)
- Where does esophageal cancer spread first?
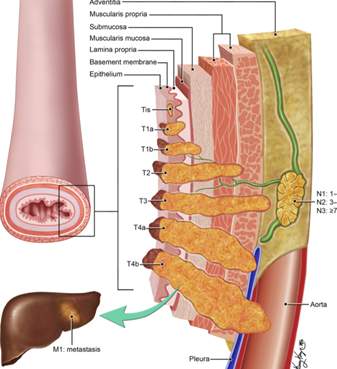
It usually spreads locally, which means invading deeper through the wall of oesophagus, then it spreads to the regional lymph node and to the distant organ.
- What are the symptoms of esophageal cancer?
Difficulty in swallowing or pain during swallowing and weight loss are the commonest symptoms of oesophageal cancer. In some patients, they have a bleeding tumour, hence leading to vomiting blood, low red cell count or passing blood through the tail end (malena).

- Does the disease have a genetic link?
For squamous cell carcinoma, it is rarely linked to genetic disease. On the other hand, around 30% of Barrett’s oesophagus and oesophageal adenocarcinoma are attributable to genetic predisposition.
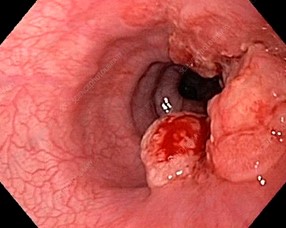
- How is esophageal cancer diagnosed?
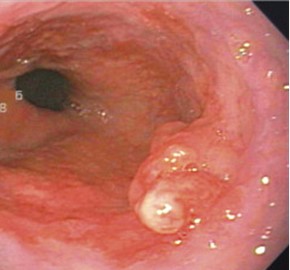
Esophageal cancer is usually diagnosed by doing an upper GI endoscopy. This involves a tube that passes through the mouth, throat then the food pipe to examine the stomach and the first segment of the small bowel.
With the advancement of technology, we are now able to detect early cancer of oesophagus better via advanced imaging. This advanced technology improves the resolution and definition of the surface and vessels of the oesophagus lining.
Once the diagnosis of oesphageal cancer is made, the patient will go through a CT scan, PET scan and /or endoscopic ultrasound for the further staging of the disease.



It is important to realize that the treatment option depends on the stage and (biological) aggressiveness of the cancer.
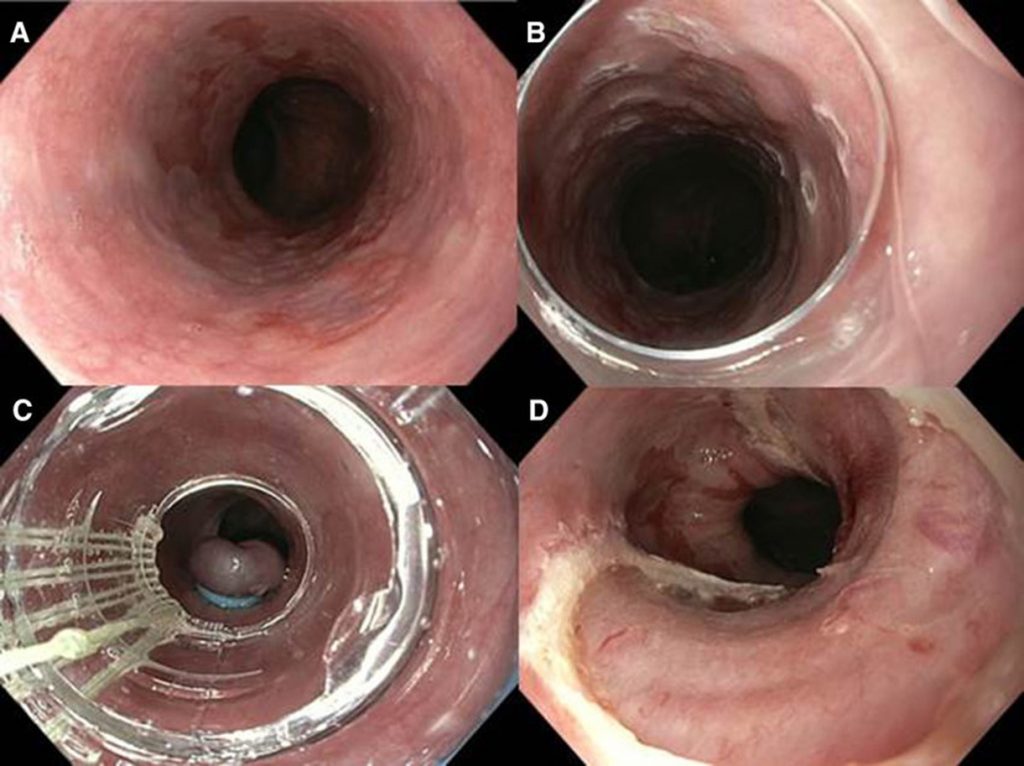
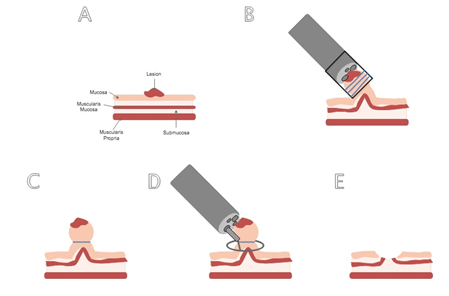
For very early cancer that is localized superficially at the lining of the oesophagus, it can be curative to remove them endoscopically. This requires an interventional endoscopist that is able to delineate the cancer and treat it endoscopically, avoiding major surgery.
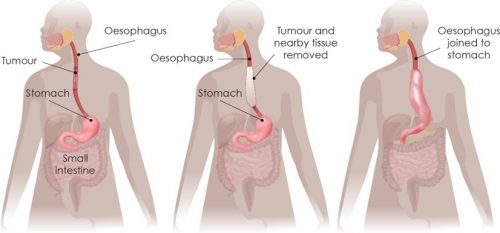
When it goes beyond the early stage, the options depend on the type and stage of the disease. In general, surgery, radiotherapy, chemotherapy and a combination of either modality are feasible depending on the condition. In particular, squamous cell carcinoma shows a good response to radiotherapy.
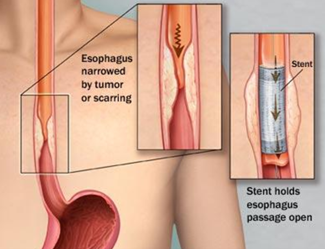
At the very late stage when the disease is advanced, we can endoscopically deploy a stent to open up the obstructed tract, so that the patient can enjoy food during palliative care period.
- Is esophageal cancer preventable by avoiding certain risk factors?
Squamous cell carcinoma is predisposed by cigarette smoking and alcohol overuse. Naturally, stopping these risk factors helps in the reduction of the risk. An interesting association between frequent hot beverage drinking with this cancer was found. Hence, frequent use of regular hot drinks such as hot tea and soup is not advisable.
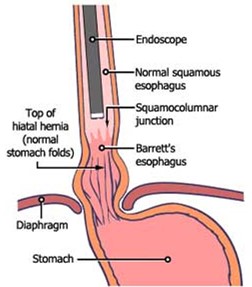
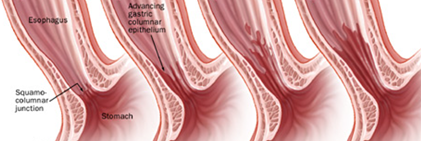
In contrast, adenocarcinoma type is strongly associated with reflux disease. Alongside genetic predisposition, the susceptible patient first develops some cell changes at the lower oesophagus lining, called Barrett’s oesophagus.
Barrett’s oesophagus is a precursor to adenocarcinoma. Hence, if one has reflux disease, the gastroenterology doctor will look for additional risk factors and decide on an endoscopy assessment. The aim is to diagnose Barrett’s oesophagus and to detect early cancer that is amenable to endoscopic treatment at an early stage, avoiding major surgery when the cancer stage is high.
We also know that obesity and smoking are modestly associated with adenocarcinoma. Again, having a healthy weight, increasing vegetable and fruit consumption, and ending cigarette usage helps to avoid the risk.
- What are the survival rates, and influencing factors with esophageal cancer?
In general, the type and stage of cancer, nutritional status and the general health of the patient play vital roles in the prognosis of the patient. Also, the cancer response to treatment such as surgery, chemotherapy and radiotherapy are equally important determinants of the success of treatment.
For example, if the patient has early cancer or even the stage before cancer – high-grade dysplasia, and had clear margin upon endoscopic resection, they have excellent cure and survival rates.
On the other hand, if a patient has aggressive cancer with stage 4 disease with poor health status, then the treatment options become limited, and they have a limited lifespan after diagnosis.
For more information about Esophageal Cancer or other medical issues, please visit www.srikotamedical.com